The Human Papillomavirus (HPV) vaccine to prevent cervical cancer will be rolled out from September 15 in Sindh, with health officials warning that social illness, sustained rumors and gaps in vaccinator training could undermine the campaign.
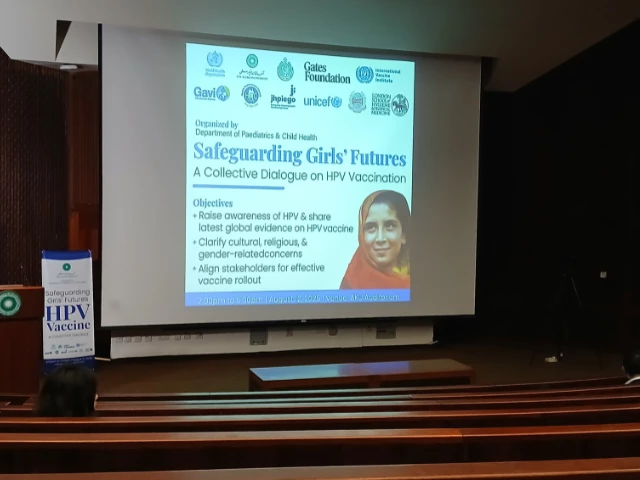
About 50% of the target audience is enrolled in schools, with coordination in progress [between health officials and the] Educational department to facilitate vaccinations at school, Dr. Rehan Baloch and spoke on the Globe HPV seminar at Aga Khan Univeristy (aku).
“We have earmarked around the RS 200 million for the HPV vaccine with further support from Gavi and other partners for advocacy and outreach,” he said, emphasizing the need for stronger commitment with parents, teachers and healthcare providers.
The campaign will trust that pediatricians, gynecologists and front -line workers will inform the local communities about HPV and the prevention of cervical cancer.
Photo courtesy: Aku
Sindh Expanded Program on Immunization (EPI) Project Director Dr. Raj Kumar described the roll -out as a “historical initiative” and said preparations were focused on operational logistics and micro planning at the Union’s advice level and drew on experience from measles, typhoid and polio campaigns.
Officials said 20 million girls aged nine to 14 are registered in schools nationwide with the rest of the school. It is estimated that 70% of vaccinations take place in schools and the rest must be administered in social settings through partnerships with public and private sectors.
What is HPV?
Cervical cancer kills more than 300,000 women all over the world each year with the heaviest death toll in countries with low and middle income. In Pakistan, the disease is among the leading cancers of women and is often diagnosed too late, despite the fact that they can be largely prevented through timely vaccination.
The human papillomavirus (HPV) – a sexually transmitted infection – is responsible for 91% of cervical cancers globally. According to the World Health Organization (WHO), more than 291 million women are diagnosed annually, and approx. 340,000 dies of the disease, most in countries like Pakistan.

The latest estimates indicate that 5,008 women in Pakistan are diagnosed with cervical cancer every year in Pakistan and 3,197 dies of the disease, according to the human papillomavirus and related cancers, factual plate 2023.
HPV has over 200 known types, classified in low risk and high risk categories. While most low-risk infections are asymptomatic and are resolved on their own, stems with high risk HPV 16 and 18 are linked to 70-80% of cases of cervical cancer. In Pakistan, nine out of 10 cases are caused by these two strains. The country reports on 5,000 new cases and 3,000 deaths each year with 73-74 million women at risk.
The HPV vaccine is most effective for girls aged nine to 14 years, but the coverage is hindered by data hulls, slow rollout and social barriers. Pakistan’s age -standardized occurrence is 6.1 per day. 100,000 women-over whos recommended threshold of four or fewer. WHO’s global strategy 2020 requires vaccination of 90% of girls in this age group by 2030, but global recording remains below 15% due to delays in national programs.
The Zekolin vaccine introduced in Pakistan protects against HPV types 16 and 18, as modeling the International Agency for Research on Cancer (IARC) suggests preventing up to 83% of cervical cancer cases in eastern Mediterranean, central, western and southern Asia. Newer generation of vaccines covering multiple HPV types could increase protection to 95%.
Top-down approach vs. community-led engagement
The success of the HPV campaign in Sindh depends not only on logistics, but also on tackling deeply rooted social inequalities. A technical, top-down approach risks alienating communities already excluded from decision-making, and emphasizes the need for participating strategies that treat local populations as equal partners of health initiatives.
Pakistan’s anchored health and education differences cannot be solved by technical corrections alone, warned Dr. Kausar’s Khan, a public health scientist and human rights activist who called for participating action research and society -driven commitment as the basis of social politics.
The country’s politics and academic elite scientists, senior bureaucrats and service providers-form a small, privileged minority, while “the poor, women, minorities, transient people and those with different sexual orientations” make up the majority, yet remains excluded from decision making, stressed Dr. Khan.
“In Karachi, more than 50% of the people of Kachhi Abadis live without water, electricity or sanitation-and anyway, we want to take science to them,” she said, warning that a science-heavy, top-down approach ignores participating ethics and local realities.
Based on his work in participating action research, Dr. Khan a “power-based, strength-based approach” that begins by “knowing yourself” and treating communities as equal partners rather than passive recipients of consciousness campaigns by focusing on women’s development department for HPV vaccination initiatives. She emphasized this, missing the campaign.
However, the assumption that vaccines and other technical interventions can tackle deeply rooted social problems is wrong.
“The successes we see are technical. But the social side is where it was,” she said, emphasizing that performance indicators and programmatic processes cannot replace the inclusion of true society.
Holes and attention
Awareness of cervical cancer and the human papillomavirus (HPV) in Pakistan remains alarmingly low, with anchored cultural norms and gender dynamics that pose major challenges for HPV vaccine recording, according to Findings from the JPEGO CAHP study presented by UNICEF’s social and behavioral change (SBC) Team.
The survey found that only 17.2% of respondents were aware of cervical cancer, only 4.4% of carers had heard of HPV, and only 2.9% knew about the existence of the HPV vaccine. UNICEF officials said that fear of cancer could be a motivator, but misunderstandings about hygiene, fatalistic beliefs and women’s limited role in the decision-making of healthcare to prevent acceptance.
Language and framing were found to have an impact on the perception – “vaccine” caused hope and prevention for young girls, while “injection” triggered a fear of needles and illness. UNICEF’s co-creation sessions emphasized to produce girls as ambitions that are rather than vulnerable objects, and using images that reflect real communities instead of idealized versions.
Awareness of the HPV vaccine is particularly low, with 95% of the people studied never heard of it. However, trust in official guidance is high – 90% said they would accept the vaccine if recommended by the government, a doctor or religious leaders. About 76-81% expressed interest in cervical cancer or HPV screening, and 79-80% said they would vaccinate themselves or their daughters.
Barriers include access to vaccines, family objections, less fear of pain or side effects, cost problems and embarrassment due to misunderstandings about the necessity of the vaccine. Reluctance is especially higher among mothers than daughters.
Mothers emerged as the most important gatekeeper for consent due to their close communication with daughters, while fathers – often not involved in daily health decisions – have passive approval that can stop campaigns.
“In fact, mothers showing a greater knowledge of cervical cancer, a more [bigger] Risk of not wanting to vaccinate their daughters compared to those who had never heard of it, “noted Dr. Fyezah Jehan, professor and chairman of AKU.” It is the trust and reassurance and addressing of these concerns that will allow us to control it better. “
She added that acceptance is highest when mothers understand both the benefits and safety of the vaccine without having general concerns about the immunization of children.
Social listening efforts from UNICEF and other partners are underway to identify local concerns and adapt communication strategies to build vaccine contract and prevent hesitation. Results show that both parents and health workers require targeted commitment.
“We need to convince our vaccinators, our health workers even more that this vaccine is good, and then they will transfer this confidence … to the communities and the most important stakeholders,” Dr. Paul Bloem, as HPV Vaccine Senior Technical Officer emphasizes the need for continuous training to strengthen confidence.
Despite strong security data, rumors persist, especially claims that associate the vaccine with infertility. Global Vaccine Safety Committee has repeatedly reviewed such claims and found “no correlation between HPV vaccination and infertility”. Experts note that the vaccine can actually help prevent infections that can reduce fertility.
Evidence from other countries, such as Bangladesh, shows that careful preparation and adoption of a one-dose strategy can achieve national coverage rates over 90% at launch. Officials warn that without similar basic work in Pakistan, high coverage from the beginning-critical of prolonged success-will remain out of reach.